In late 2025, the United States introduced one of its most sweeping changes to immigration policy in decades. The U.S. Department of State issued an internal directive instructing consular officers around the world to evaluate visa applicants’ health more aggressively than ever before. For the first time, obesity was listed as a potential basis for denial, along with chronic illnesses such as diabetes, cancer, mental health disorders, respiratory diseases, and cardiovascular conditions. The change, implemented under President Donald Trump’s administration, was presented as an effort to reduce long-term financial strain on American taxpayers. Almost immediately, it ignited a nationwide debate, with supporters praising its fiscal logic and critics warning that it opened the door to discrimination.
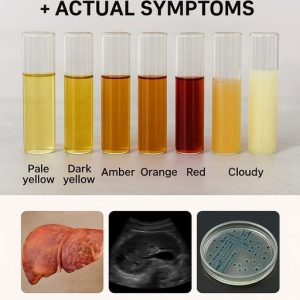
This directive represented a significant expansion of the “public charge” principle, which has historically evaluated whether immigrants might rely on government assistance. Previously, decisions focused more on financial stability, income, or the likelihood of depending on welfare benefits. Under the new guidance, however, the definition broadened to include health-related financial risk. Consular officers were instructed to assess whether an applicant’s medical condition could result in substantial long-term costs to the U.S. government. Officers were told to consider the potential price of hospital visits, chronic disease management, long-term care, medications, and emergency treatments. Even applicants with steady income or established careers could face denial if their health conditions suggested future expenses.
The policy is expected to affect immigrant visa applicants most significantly—especially those applying for permanent residency. Family-sponsored immigrants, who rely on financial sponsors, could be particularly vulnerable, since sponsors may not be able to guarantee coverage for extensive medical needs. Employment-based applicants, including highly skilled workers, may also face hurdles if they have chronic conditions deemed costly. Temporary visitors such as tourists and business travelers will still be reviewed, but officers are instructed to prioritize scrutiny for long-term immigrants. Legal experts predict the new rule will lead to more visa refusals, longer wait times, increased appeals, and major court battles.
Immigration attorneys quickly criticized the policy, arguing that consular officers are not medical professionals and cannot accurately evaluate complex health issues. Charles Wheeler of the Catholic Legal Immigration Network stated that officers lack the training to assess risks fairly or consistently. He and other experts warned that subjective judgment could lead to unequal outcomes, varying widely between embassies. They also argued that the rule conflicts with the longstanding Foreign Affairs Manual, which emphasized objective, evidence-based criteria. Critics believe the rule could encourage discrimination based on body size, disability, or socioeconomic background—given that factors like obesity are often heavily shaped by environment, genetics, and cultural conditions.
Public health researchers joined the chorus of concern, noting that obesity and many chronic illnesses are not simply matters of personal choice. In many countries, nutritious food is scarce or expensive, healthcare access is limited, and cultural factors influence diet and activity. Treating obesity as grounds for rejecting immigrants, they argued, ignores these complexities and risks stigmatizing millions of people. Mental health advocates added that including conditions such as anxiety or depression could deepen stigma and unfairly penalize applicants who live with manageable conditions. These organizations fear the policy could separate families, disproportionately affect applicants from developing nations, and violate international principles of equal treatment.
Supporters of the directive, however, defended it as a practical and necessary reform. Conservative commentators described it as an act of “responsible budgeting,” one that protects American taxpayers from inheriting the medical costs of newcomers. They argue that wealthier countries must evaluate whether they can sustainably welcome immigrants who may require extensive medical care. Policymakers who support the rule say it is consistent with earlier public charge interpretations, claiming it simply modernizes the criteria to reflect current healthcare expenses. To these supporters, the policy ensures fairness, both to taxpayers and to immigrants who arrive prepared to support themselves financially.
The new rule also triggered a wave of global reactions. Social media erupted with debate, with some users calling the policy discriminatory while others applauded its economic logic. Prospective immigrants, especially those planning to join family members in the United States, expressed fear and confusion. Many wondered whether mild obesity or controlled chronic conditions could jeopardize their applications. Doctors in multiple countries questioned how officers would define obesity and whether they would use BMI or merely visual judgment. Because the directive did not include clear measurement tools or medical standards, uncertainty only increased.
Humanitarian organizations strongly condemned the changes, warning that they could divide families and create a two-tier immigration system—one for the healthy and one for those deemed a “risk.” They argued that the rule ignores ethical principles that view migration as a human right and that it disproportionately punishes individuals for medical conditions often beyond their control. Families applying for visas worry they may face delays, denial, or the need to gather extensive medical documentation. Some may be required to obtain new insurance, secure additional financial sponsorship, or undergo new medical evaluations, adding complexity and cost to an already difficult process.
Looking ahead, the long-term consequences of the policy remain uncertain. If the directive stays in place, experts predict a reduction in immigration, especially from countries with high rates of obesity or chronic disease. Skilled workers may choose to pursue opportunities in more inclusive countries, while families may face painful separations. Some economists caution that industries dependent on immigrant labor could experience shortages. Because the policy was introduced through internal guidance rather than through formal regulation or legislation, it can be overturned by future administrations. Legal challenges may also threaten its continuation, as advocacy groups prepare to contest the rule in court.
For now, the directive marks a major shift in U.S. immigration philosophy, moving the focus from traditional security concerns to personal health. While supporters hail it as fiscally responsible, critics argue it is discriminatory, medically unsound, and ethically troubling. What remains clear is that the rule will affect millions worldwide—from applicants preparing to enter the U.S. to families waiting anxiously for reunification. The future of the policy will depend on political decisions, legal rulings, and public response, but its immediate impact has already reshaped the global immigration landscape.