Gynecological appointments are one of the most important — and often most misunderstood — parts of preventive healthcare. For many women, these visits can bring up feelings of anxiety, vulnerability, embarrassment, or even fear. Yet they remain essential for early detection of serious conditions, routine screening, reproductive health management, and overall well-being.
Understanding why these appointments matter, what to expect, and how to make them more comfortable can transform the experience from something stressful into something empowering.
Why Gynecological Care Matters
Routine gynecological exams are designed to detect issues before symptoms become severe. Early identification of cervical changes through Pap tests can prevent cervical cancer. Breast exams can help detect abnormalities at an early stage. Screenings for sexually transmitted infections (STIs) protect both individual and partner health. Hormonal discussions can uncover imbalances that affect mood, sleep, fertility, and long-term bone health.
Preventive care is far more effective than reactive care. Many serious reproductive health conditions develop silently. Regular visits allow healthcare providers to monitor subtle changes over time, creating a clearer picture of your overall health.
Even if you feel completely healthy, routine exams provide reassurance and baseline measurements for the future. They also create a trusted relationship with a provider — someone you can turn to if new symptoms arise.
Understanding Common Fears
Despite the clear medical benefits, emotional barriers often prevent women from scheduling appointments. Some common concerns include:
• Feeling exposed or physically vulnerable
• Worry about body image or grooming
• Fear of pain during the exam
• Anxiety about receiving bad news
• Previous negative healthcare experiences
• Cultural or personal modesty concerns
All of these feelings are valid. A gynecological exam is intimate. It requires trust. Recognizing that anxiety is normal is the first step toward managing it.
It’s important to remember that gynecologists are trained medical professionals. They perform pelvic exams, breast exams, and screenings every day. Their focus is medical — not cosmetic. Whether you shaved, waxed, or did nothing at all is medically irrelevant. Your provider is concerned with tissue health, not appearance.
Preparing for Your Appointment
Preparation can reduce anxiety significantly. When you feel ready and informed, you regain a sense of control.
-
Schedule Thoughtfully
If possible, schedule your appointment for a time when you are not rushed. Avoid planning it on an already stressful day. Give yourself space before and after the visit. -
Hygiene — Keep It Simple
Showering beforehand can help you feel more confident. However, avoid scented soaps, douches, vaginal sprays, or powders. The vagina is self-cleaning, and these products can disrupt its natural balance. They may also affect test accuracy.
If you are menstruating, many clinics will still proceed with the appointment. Inform the office when scheduling if you are unsure.
-
Dress Comfortably
Loose, easy-to-remove clothing can make the process smoother. A dress or long top may help you feel less exposed when changing. Comfortable underwear can also make a difference in how relaxed you feel before the exam. -
Write Down Questions
It’s common to forget concerns once you’re in the exam room. Write down symptoms, cycle irregularities, pain patterns, discharge changes, or emotional concerns. No issue is “too small” to mention. -
Consider Emotional Support
If allowed, you may bring a trusted friend or partner to wait in the lobby. Knowing someone supportive is nearby can ease anxiety.
What Happens During a Typical Visit
Understanding the process removes uncertainty — and uncertainty often fuels fear.
Medical History Discussion
Your provider will ask about menstrual cycles, sexual activity, birth control, pregnancies, family medical history, medications, and any symptoms you’ve noticed. Honesty is crucial. Providers are not there to judge; they are there to diagnose and treat accurately.
Breast Exam
The provider may manually check for lumps or abnormalities. You may also receive guidance on self-exams.
Pelvic Exam
During the pelvic exam, you’ll lie back with your feet in footrests. A speculum is gently inserted to allow visualization of the cervix. A Pap test may be performed, which involves collecting cervical cells for analysis. You may feel pressure, but it should not be sharply painful. If it is, speak up immediately.
Bimanual Exam
The provider may use gloved fingers to feel internal organs (uterus and ovaries) for size, shape, or tenderness.
The entire physical portion is usually brief. Communicating discomfort in real time allows adjustments to be made.
How to Reduce Discomfort
• Practice slow, deep breathing before and during the exam.
• Ask the provider to explain each step before it happens.
• Request a smaller speculum if you are sensitive.
• Relax your abdominal and pelvic muscles consciously.
• Tell the provider if you have a history of trauma — this allows them to proceed more gently and mindfully.
You have the right to pause the exam at any time.
Communication Is Power
One of the most important aspects of gynecological care is open dialogue. If you feel nervous, say so. If something hurts, speak up. If you prefer a provider of a certain gender, request one. If you want a nurse present, ask.
Healthcare is collaborative. You are not passive in the process.
If you’ve had a negative experience in the past, consider trying a different provider. A supportive, respectful gynecologist can make an enormous difference in comfort levels.
Special Situations
First Appointment
The first visit may feel intimidating. Remember, it is often mostly discussion. Exams are tailored based on age and medical need.
After Childbirth
Postpartum visits are essential for healing assessment, hormonal evaluation, and emotional well-being screening.
Menopause
Hormonal changes can cause dryness, discomfort, sleep issues, and mood shifts. Gynecologists provide solutions and guidance during this transition.
Sexual Health Concerns
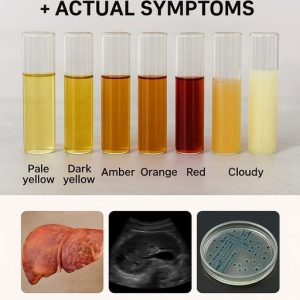
Pain during intercourse, low libido, unusual discharge, itching, or odor are medical concerns — not sources of shame.
Trauma Survivors
If you have a history of sexual trauma, inform your provider beforehand. Trauma-informed care allows slower pacing, consent at every step, and greater sensitivity.
The Psychological Side of Avoidance
Avoiding appointments may temporarily reduce anxiety, but it increases long-term risk. Fear of bad news is common, yet early detection dramatically improves outcomes in most gynecological conditions.
Often, anxiety decreases significantly after the appointment is over. Many women report relief and pride afterward.
Reframing the Visit
Instead of viewing the appointment as something being “done to you,” consider it something you are choosing for yourself. It is an act of self-protection, self-respect, and long-term planning.
Preventive care is proactive strength.
Building a Healthy Routine
• Schedule annual exams at the same time each year.
• Track menstrual cycles and symptoms in a journal or app.
• Maintain open communication with your provider between visits if new symptoms arise.
• Stay informed about recommended screenings for your age group.
The Role of Trust
Trust builds over time. If your current provider makes you feel rushed or dismissed, it is appropriate to seek another. Feeling heard and respected is not optional — it is fundamental.
A supportive gynecologist will:
• Listen without interrupting
• Explain procedures clearly
• Ask for consent before proceeding
• Encourage questions
• Respect your boundaries
Your Comfort Matters
Small adjustments can make big differences:
• Warm socks during the exam
• Requesting a sheet for additional coverage
• Listening to calming music beforehand
• Scheduling morning appointments to avoid all-day anxiety
You deserve comfort and dignity during medical care.
Long-Term Benefits
Regular gynecological visits help:
• Detect cervical changes early
• Monitor ovarian health
• Address fertility concerns
• Screen for infections
• Manage hormonal conditions
• Identify breast abnormalities
• Provide contraception guidance
• Offer menopause support
Preventive healthcare is an investment in decades of future well-being.
A Final Encouraging Thought
It is understandable to feel vulnerable during intimate medical care. But vulnerability in a medical setting is not weakness — it is courage. Each appointment represents a choice to prioritize your health.
Approach your next visit not with dread, but with the understanding that you are taking control of your future. You are not alone in your anxiety. Millions of women share similar feelings, yet continue to show up for themselves year after year.
Gynecological care is not about embarrassment or judgment. It is about protection, prevention, and peace of mind.
Your body deserves attentive care. Your concerns deserve to be heard. And your health is worth every moment of temporary discomfort.
Disclaimer: This article provides general health information and is not a substitute for professional medical advice. Always consult a qualified healthcare provider regarding personal medical concerns or symptoms.